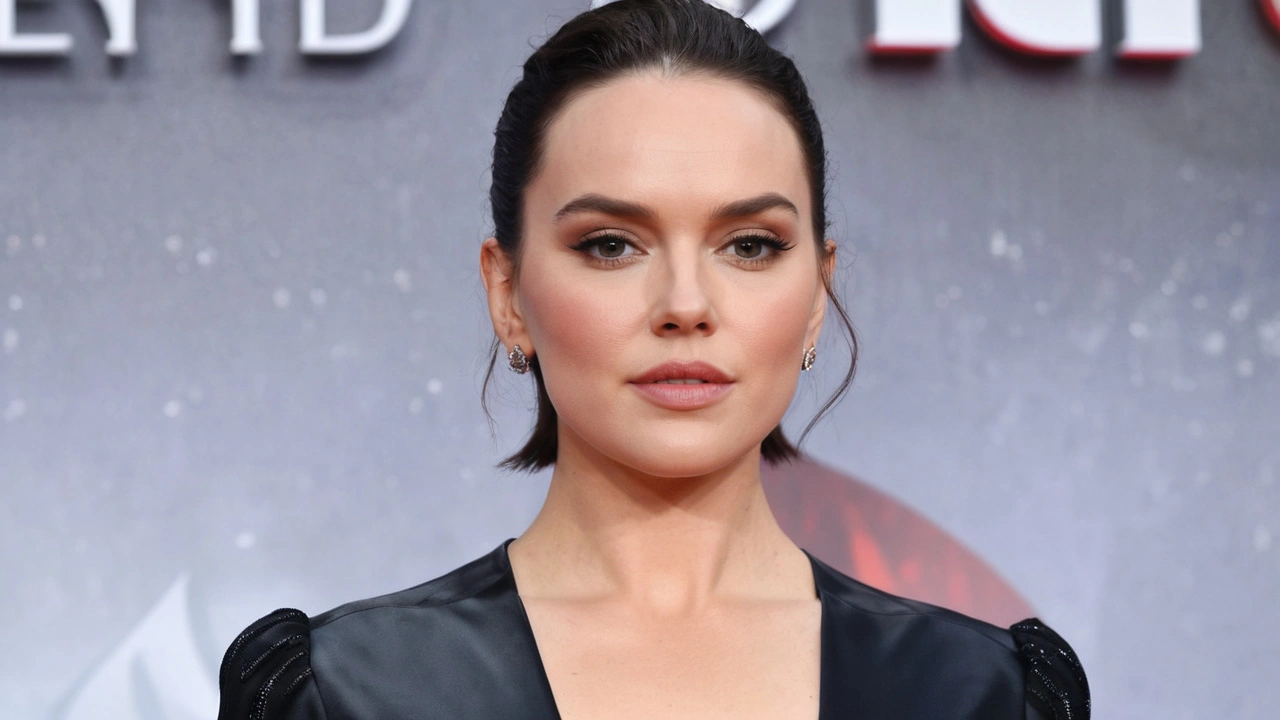
Daisy Ridley Opens Up About Her Graves' Disease Diagnosis and Recovery Journey
Daisy Ridley, who captivated audiences worldwide with her portrayal of Rey in the Star Wars franchise, has recently opened up about a personal health struggle that has been affecting her for months. In September 2023, Ridley received a diagnosis of Graves' disease, an autoimmune disorder that leads the thyroid to overproduce hormones. This condition, which often goes misdiagnosed or undiscovered for an extended period, causes a variety of disruptive and challenging symptoms.
Recognizing the Signs
Ridley's journey to diagnosis began with a slew of uncomfortable and perplexing symptoms. Initially, she believed that her racing heart, significant weight loss, and overwhelming exhaustion were due to the physical and mental stress of embarking on a particularly demanding film project. It wasn’t until her doctor suspected that her symptoms might be linked to something more severe, namely Graves' disease, that she got closer to understanding her condition.
The range of symptoms she experienced also included tremors in her hands, making it difficult at times to even hold a pen. Emotional irritability was another significant symptom, transforming her usual demeanor and making interpersonal interactions more challenging. For Ridley, these experiences underscored the imperative that individuals should never normalize feeling unwell or dismiss their health concerns.
A Personal Revelation
Upon reflection, Ridley admits that the diagnosis came as both a shock and a relief. On the one hand, it confirmed that her debilitating symptoms were not just in her imagination. On the other, it provided a concrete path forward toward managing her health. She has since become vocal about the importance of proper diagnosis and treatment for conditions like Graves' disease, which is still relatively unheard of by the general public.
Ridley's transparency about her experience aims to bring awareness to the condition that predominantly affects young and middle-aged women. Moreover, she hopes to encourage others to seek medical advice when experiencing unexplained health issues. According to her, the first step towards recovery is recognizing that something is genuinely wrong and needs addressing.
Adjusting to a New Lifestyle
Post-diagnosis, Ridley has had to make several significant lifestyle and dietary adjustments to regain control over her health. She now follows a balanced diet free of foods that can exacerbate thyroid problems. Additionally, she has incorporated regular exercise into her routine to maintain her physical and mental well-being. These changes have proven transformative, dramatically improving her quality of life.
She also highlights the importance of stress management, noting that sustained stress can have a profound impact on the body, particularly for those dealing with autoimmune disorders. Implementing relaxation techniques, such as yoga and meditation, has become an integral part of her daily routine.
Living with Graves' Disease
Living with Graves' disease requires ongoing management and medical supervision. Ridley’s experience is a reminder of the complexities involved in dealing with autoimmune disorders. The symptoms can vary widely and may affect each individual differently. Common manifestations include nervousness, heightened perspiration, muscle weakness, difficulty sleeping, and increased bowel movements. In some cases, women with Graves' disease might experience lighter or even absent menstrual periods.
Ridley stresses the importance of raising public awareness about this condition. Early detection is key to preventing severe complications, which can include vision problems or even cardiovascular issues if left untreated. By speaking openly about her journey, she hopes to lessen the stigma and misinformation surrounding Graves' disease.
The Bigger Picture
Graves' disease impacts an estimated 2-3% of the population, with a significant number of cases being undiagnosed. Family history and smoking are among the risk factors associated with the disorder. In this context, Ridley’s story serves as a significant reminder of the crucial role that awareness and early intervention play in handling autoimmune diseases.
Healthcare professionals emphasize that if someone shows symptoms akin to those Ridley experienced, they should seek medical advice promptly. Standard treatments for Graves' disease include antithyroid medications, radioactive iodine therapy, or surgery in more severe cases. Lifestyle modifications and stress management also play substantial roles in managing the condition.
Charting the Path Ahead
As Ridley continues her journey towards health, she remains optimistic about her future. She is committed to maintaining the lifestyle changes that have benefited her thus far. Her resilience and determination serve as an inspiration to many, highlighting the importance of prioritizing health and well-being amidst a demanding career.
In sharing her story, Ridley hopes to ignite conversations around autoimmune disorders, encouraging more people to listen to their bodies and seek the care they need. Her message is clear: feeling unwell should never be brushed off as normal, and seeking medical advice is crucial for addressing underlying health issues.
Ridley's openness about her diagnosis and the steps she has taken to manage it provides a valuable perspective on living with Graves' disease. As the conversation around autoimmune disorders grows, her story will undoubtedly play a part in guiding and supporting others facing similar challenges.

Comments
pradeep kumar
Your post is just another self‑pity parade disguised as inspiration.
August 7, 2024 at 18:42
love monster
Thanks for shedding light on Daisy's journey; it’s a solid case study of how autoimmune dysregulation can cascade into psychosomatic load. The way you outlined the thyroid hormone feedback loop was spot on, and the emphasis on lifestyle integration is a pragmatic blueprint for anyone navigating similar health vectors. Keep stacking that evidence‑based discourse, it really helps the community calibrate their own recovery protocols.
August 7, 2024 at 19:33
Christian Barthelt
While the article is well‑meaning, it suffers from a plethora of linguistic and factual missteps that deserve scrutiny. First, the opening paragraph mistakenly uses the phrase “overproduce hormones” without the requisite hyphen, which undermines its scientific credibility. Second, the description of Graves' disease as merely “autoimmune” neglects the nuance of TSH‑receptor antibodies, a detail any endocrinology textbook would highlight. Third, the piece conflates “weight loss” with “significant” without quantifying what constitutes a clinically relevant change; this is a classic case of vague terminology. Fourth, the claim that stress management can “dramatically improve” quality of life lacks citation – a blanket statement that borders on hyperbole. Fifth, the article mentions “radioactive iodine therapy” as a treatment but fails to address its potential side‑effects, such as hypothyroidism, which is essential information for informed consent. Sixth, the timeline of Daisy’s diagnosis is presented ambiguously; readers are left to infer whether the symptoms spanned weeks or months. Seventh, the piece incorrectly states that Graves' disease “might cause lighter or even absent menstrual periods,” ignoring the broader endocrine interactions that can also alter cycle length. Eighth, the use of the term “autoimmune disorder” repeatedly without specifying the immunopathology feels like filler. Ninth, the article’s structure jumps from personal anecdote to epidemiology without a transitional sentence, creating a jarring narrative flow. Tenth, the mention of “balanced diet free of foods that can exacerbate thyroid problems” is overly simplistic – not all patients respond identically to dietary changes, and no specific macronutrient guidance is offered. Eleventh, the section on “stress management” suggests yoga and meditation as panaceas, yet neglects evidence‑based cognitive behavioral strategies that have stronger empirical support. Twelfth, the piece omits any discussion of beta‑blockers, a common pharmacologic option for symptomatic relief. Thirteenth, the assertion that “early detection is key to preventing severe complications” is true, but the article fails to enumerate those complications beyond vague references to vision and cardiovascular issues. Fourteenth, the final paragraph’s call to “listen to their bodies” is clichéd and adds little substantive value. Fifteenth, the overall tone oscillates between reverent fan‑fare and quasi‑medical report, leaving the reader uncertain about the article’s primary intent. In sum, the narrative would benefit from stricter editorial standards, precise medical terminology, and more rigorous source attribution.
August 7, 2024 at 21:46
Ify Okocha
Daisy's transparency is commendable, yet the article glosses over the metabolic cascade that underlies her symptoms. The tremors and irritability are classic manifestations of heightened beta‑adrenergic activity, which warrants a detailed look at sympathetic overdrive. Moreover, the claim that a “balanced diet” resolves thyroid dysregulation is misleading; macronutrient distribution, iodine intake, and selenium status all play critical roles. Stress reduction techniques are beneficial, but without quantifiable metrics, readers are left guessing about efficacy. In short, the piece could have delved deeper into pathophysiology rather than staying at a superficial level.
August 7, 2024 at 23:10
William Anderson
Interesting perspective, but the analysis feels half‑baked. The article’s headline promises an in‑depth recovery roadmap, yet the content skims over the therapeutic nuances. A more rigorous breakdown of medication titration schedules, monitoring of free T4 levels, and side‑effect profiling would have elevated the discussion. As it stands, the narrative is more mood‑piece than substantive guide.
August 8, 2024 at 00:33